Judge Digs Into Medicaid Contract Disputes
A legal showdown over contracts in Florida's multibillion-dollar Medicaid program started Monday in an administrative court.The stakes are high…
August 28, 2018 at 04:41 PM
4 minute read
 Photo courtesy of kenary820/Shutterstock
Photo courtesy of kenary820/Shutterstock
A legal showdown over contracts in Florida's multibillion-dollar Medicaid program started Monday in an administrative court.
The stakes are high as the state prepares to transition Medicaid managed-care patients to new plans chosen in the latest round of contracting.
In a small courtroom a mile down the road from the state Capitol, attorneys for the AIDS Healthcare Foundation and two South Florida hospital districts asked a judge to either require new bids or to award new contracts in a dispute about what are known as “specialty” contracts in the Medicaid managed-care system.
A subsidiary of the AIDS Healthcare Foundation and the South Florida Community Care Network, jointly owned by the hospital districts, filed the challenges after they were denied contracts.
The attorneys told Administrative Law Judge John Newton that, among other things, the state didn't assign enough staff to properly evaluate the plans' responses to the Medicaid managed-care invitation to negotiate and, as a result, they weren't properly scored. An invitation to negotiate, or ITN, is a bid-like process often used by government agencies.
AIDS Healthcare Foundation attorney Brian Newman pointed to the staffing problems. While there were more than 67,000 items that plans were required to respond to, Newman alleged that AHCA at the last minute removed some items from review because of lack of time.
“When they say that all the scoring was completed that's only half true,” Newman said. “The scoring was completed only because they reduced the number of items that had to be scored.”
The South Florida Community Care Network, jointly owned by the North Broward and South Broward hospital districts, also argued that state law requires AHCA to contract with so-called “provider sponsored networks” when possible.
The new contracts have the potential to upend health care for HIV and AIDS patients in South Florida who are members of Positive Health Care, the managed-care plan owned by the AIDS Healthcare Foundation.
But attorneys for the Agency for Care Administration argued that the ITN, like sports, is competitive, with winners and losers.
“It's not a game, but it is a competition,” said Joe Goldstein, an attorney with the firm Shutts & Bowen who is representing the state.
AHCA has gone through a lengthy re-procurement process that starred in 2017 to award new contracts. Initially, the state announced in April that it would sign five-year Medicaid contracts with nine managed care plans. The initial announcement drew the threat of legal challenges from a number of plans.
AHCA eventually negotiated agreements with an additional four companies, announcing this summer that it would sign five-year contracts with 13 managed care plans. But the decision still left Positive Health Care shut out of Broward and Miami Dade counties.
And while the South Florida Community Care Network, which operates as Community Care Network, was picked to provide so-called “managed medical assistance” or traditional health care to people in Broward County, it wasn't chosen by the state to provide specialty care to people with HIV, people with serious mental illness or children with special health care needs.
The challenges, along with cases filed by Magellan Complete Care about providing care to people with mental illness, were consolidated into one case. Newton began hearing the case Monday.
But in lieu of an opening statement, Tallahassee attorney Steve Ecenia announced that Magellan Complete Care was voluntarily dismissing its challenges. Details were not immediately available, but a settlement agreement will include a Medicaid award for Magellan, Ecenia told The News Service of Florida.
The settlement agreement won't impact the challenges filed by the AIDS Healthcare Foundation and the South Florida Community Care Network.
State lawmakers in 2011 approved an overhaul of the Medicaid program that requires most beneficiaries to enroll in HMOs or other types of managed-care plans.
AHCA launched the program in 2013 after signing five-year contracts with health plans across the 11 regions. It began reprocurement efforts in 2017, issuing an invitation to negotiate with managed-care plans that want new five-year contracts.
After months of reviews and negotiations AHCA announced the 13 managed care plans it intends to contract with. In aggregate, the five-year contracts are expected to be worth about $90 billion, one top-ranking Medicaid official has said. That number could be low, though, because the program, which provides health care to more than 3.2 million Floridians, has cost the state more than $25 billion annually.
Christine Sexton reports for the News Service of Florida.
This content has been archived. It is available through our partners, LexisNexis® and Bloomberg Law.
To view this content, please continue to their sites.
Not a Lexis Subscriber?
Subscribe Now
Not a Bloomberg Law Subscriber?
Subscribe Now
NOT FOR REPRINT
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.
You Might Like
View All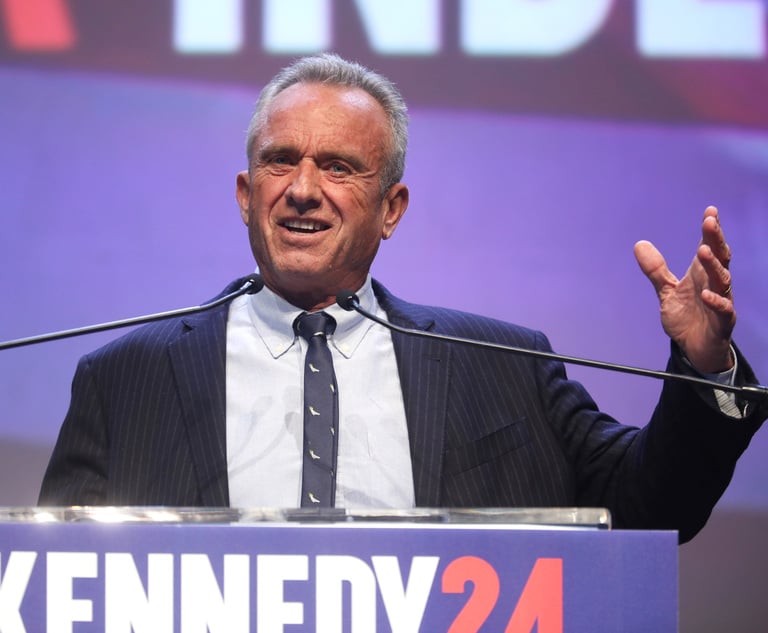
RFK Jr. Will Keep Affiliations With Morgan & Morgan, Other Law Firms If Confirmed to DHHS
3 minute read
Attorneys, Health Care Officials Face Nearly $80M RICO Suit Over Allegedly Fabricated Spreadsheet


Amid Growing Litigation Volume, Don't Expect UnitedHealthcare to Change Its Stripes After CEO's Killing
6 minute readTrending Stories
Who Got The Work
J. Brugh Lower of Gibbons has entered an appearance for industrial equipment supplier Devco Corporation in a pending trademark infringement lawsuit. The suit, accusing the defendant of selling knock-off Graco products, was filed Dec. 18 in New Jersey District Court by Rivkin Radler on behalf of Graco Inc. and Graco Minnesota. The case, assigned to U.S. District Judge Zahid N. Quraishi, is 3:24-cv-11294, Graco Inc. et al v. Devco Corporation.
Who Got The Work
Rebecca Maller-Stein and Kent A. Yalowitz of Arnold & Porter Kaye Scholer have entered their appearances for Hanaco Venture Capital and its executives, Lior Prosor and David Frankel, in a pending securities lawsuit. The action, filed on Dec. 24 in New York Southern District Court by Zell, Aron & Co. on behalf of Goldeneye Advisors, accuses the defendants of negligently and fraudulently managing the plaintiff's $1 million investment. The case, assigned to U.S. District Judge Vernon S. Broderick, is 1:24-cv-09918, Goldeneye Advisors, LLC v. Hanaco Venture Capital, Ltd. et al.
Who Got The Work
Attorneys from A&O Shearman has stepped in as defense counsel for Toronto-Dominion Bank and other defendants in a pending securities class action. The suit, filed Dec. 11 in New York Southern District Court by Bleichmar Fonti & Auld, accuses the defendants of concealing the bank's 'pervasive' deficiencies in regards to its compliance with the Bank Secrecy Act and the quality of its anti-money laundering controls. The case, assigned to U.S. District Judge Arun Subramanian, is 1:24-cv-09445, Gonzalez v. The Toronto-Dominion Bank et al.
Who Got The Work
Crown Castle International, a Pennsylvania company providing shared communications infrastructure, has turned to Luke D. Wolf of Gordon Rees Scully Mansukhani to fend off a pending breach-of-contract lawsuit. The court action, filed Nov. 25 in Michigan Eastern District Court by Hooper Hathaway PC on behalf of The Town Residences LLC, accuses Crown Castle of failing to transfer approximately $30,000 in utility payments from T-Mobile in breach of a roof-top lease and assignment agreement. The case, assigned to U.S. District Judge Susan K. Declercq, is 2:24-cv-13131, The Town Residences LLC v. T-Mobile US, Inc. et al.
Who Got The Work
Wilfred P. Coronato and Daniel M. Schwartz of McCarter & English have stepped in as defense counsel to Electrolux Home Products Inc. in a pending product liability lawsuit. The court action, filed Nov. 26 in New York Eastern District Court by Poulos Lopiccolo PC and Nagel Rice LLP on behalf of David Stern, alleges that the defendant's refrigerators’ drawers and shelving repeatedly break and fall apart within months after purchase. The case, assigned to U.S. District Judge Joan M. Azrack, is 2:24-cv-08204, Stern v. Electrolux Home Products, Inc.
Featured Firms
Law Offices of Gary Martin Hays & Associates, P.C.
(470) 294-1674
Law Offices of Mark E. Salomone
(857) 444-6468
Smith & Hassler
(713) 739-1250






