Lawmakers Weigh Requiring 500,000 Medicaid Beneficiaries to Work
Members of a House health care panel this week approved HB 955, which is now ready to go to the full House.
April 11, 2019 at 12:39 PM
5 minute read
 Rep. Daniel Perez. Photo courtesy of the Florida House of Representatives.
Rep. Daniel Perez. Photo courtesy of the Florida House of Representatives.Florida lawmakers are considering requiring an estimated 500,000 Medicaid beneficiaries to work or show they are trying to get jobs to keep their health care benefits, despite recent court rulings that have struck down similar requirements.
Members of a House health care panel this week approved the proposal (HB 955), which is now ready to go to the full House.
While the Senate hasn't considered the proposal this legislative session, the notion of a work requirement is supported by Sen. Aaron Bean, a Fernandina Beach Republican in charge of crafting the Senate's health care spending plan.
“I would be interested in that,” Bean said when asked about the issue.
The House is moving forward with the legislation after a pair of rulings by U.S. District Judge James E. Boasberg that tossed similar work requirements in Kentucky and Arkansas. Boasberg serves in the District of Columbia.
Mandating work requirements has been a long-standing priority for conservatives. In a party-line vote, members of the House Health and Human Services Committee on Tuesday approved the Florida bill, sponsored by Rep. Daniel Perez, R-Miami.
The proposed work requirement would hit low-income adults who have children.
“The true intent of this bill really is good at heart. It's just to make sure that the individuals who are able to work, that are able to get back to our society, are doing so if they are receiving government benefits,” Perez said.
But Joan Alker, executive director of the Center for Children and Families at Georgetown University, disagreed.
“If this bill becomes law, it would be the harshest (and that is saying something!) that I have seen so far — with no parent excluded unless they have a newborn under 3 months old,” Alker wrote in her blog, describing the bill.
Florida has the fourth-largest Medicaid program in the nation in terms of the number of beneficiaries and the fifth-largest program in terms of expenditures, according to state Medicaid officials. The program covers nearly 4 million people — mostly through Medicaid managed care plans — and costs more than $28 billion.
Not all low-income people in Florida qualify for the Medicaid program. The state determines eligibility, and lawmakers have set different eligibility requirements for different groups.
For instance, pregnant women can earn almost twice as much as the poverty level, which is $12,140 for an individual, and be enrolled in the Medicaid program. Florida has not expanded Medicaid to able-bodied childless adults.
The House bill would direct the Agency for Health Care Administration to request federal approval to require beneficiaries to engage in work activities to remain eligible for Medicaid coverage. The bill would exempt people who receive Medicaid long-term care coverage, such as seniors in nursing homes.
The proposed work activities mirror those already included in a state temporary cash assistance program. Florida requires the maximum number of work hours allowed under federal law, which means, for example, that single parents with children over age 6 are required to work 30 hours per week.
The proposed Medicaid work requirements would not apply to the large number of children who receive health care through the program and are not expected to apply to people who qualify for Social Security Disability Income.
Katie Betta, a spokeswoman for Senate President Bill Galvano, R-Bradenton, said in an email Wednesday that Galvano is “open to work requirements for able-bodied adults.” But she said his support in the past for such ideas also involved wanting options to meet the requirements, including on-the-job training, job-placement activities and pursuit of educational opportunities. She also said he has wanted exceptions for people with disabilities and caregivers of people with disabilities.
Karen Woodall, a longtime social-services lobbyist, told House committee members that Medicaid and the temporary cash assistance programs aren't the same. One program provides money, she said, while the other provides health benefits.
Requiring Medicaid beneficiaries to work would likely result in people losing coverage, said Woodall, executive director of the left-leaning Florida Center for Fiscal and Economic Policy.
Also, the jobs Medicaid enrollees are able to secure may not come with benefits such as health insurance, she said, adding that would leave them with little money and no health care coverage.
“I would encourage you to look at a different approach in assisting the folks and see what kind of help can be there without tying loss of their health insurance to it, because you are just going to exacerbate the loss of their health insurance to it,” Woodall said.
Christine Sexton reports for the News Service of Florida.
This content has been archived. It is available through our partners, LexisNexis® and Bloomberg Law.
To view this content, please continue to their sites.
Not a Lexis Subscriber?
Subscribe Now
Not a Bloomberg Law Subscriber?
Subscribe Now
NOT FOR REPRINT
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.
You Might Like
View All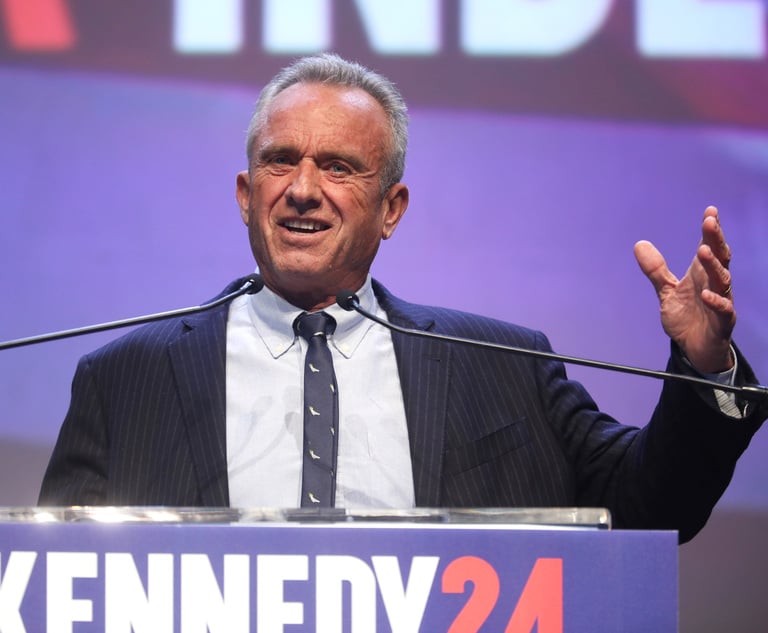
RFK Jr. Will Keep Affiliations With Morgan & Morgan, Other Law Firms If Confirmed to DHHS
3 minute read
Attorneys, Health Care Officials Face Nearly $80M RICO Suit Over Allegedly Fabricated Spreadsheet


Amid Growing Litigation Volume, Don't Expect UnitedHealthcare to Change Its Stripes After CEO's Killing
6 minute readTrending Stories
- 1Roundup Special Master's Report Recommends Lead Counsel Get $0 in Common Benefit Fees
- 2Georgia Justices Urged to Revive Malpractice Suit Against Retired Barnes & Thornburg Atty
- 3How Gibson Dunn Lawyers Helped Assemble the LA FireAid Benefit Concert in 'Extreme' Time Crunch
- 4Lawyer Wears Funny Ears When Criticizing: Still Sued for Defamation
- 5Medical Student's Error Takes Center Stage in High Court 'Agency' Dispute
Who Got The Work
J. Brugh Lower of Gibbons has entered an appearance for industrial equipment supplier Devco Corporation in a pending trademark infringement lawsuit. The suit, accusing the defendant of selling knock-off Graco products, was filed Dec. 18 in New Jersey District Court by Rivkin Radler on behalf of Graco Inc. and Graco Minnesota. The case, assigned to U.S. District Judge Zahid N. Quraishi, is 3:24-cv-11294, Graco Inc. et al v. Devco Corporation.
Who Got The Work
Rebecca Maller-Stein and Kent A. Yalowitz of Arnold & Porter Kaye Scholer have entered their appearances for Hanaco Venture Capital and its executives, Lior Prosor and David Frankel, in a pending securities lawsuit. The action, filed on Dec. 24 in New York Southern District Court by Zell, Aron & Co. on behalf of Goldeneye Advisors, accuses the defendants of negligently and fraudulently managing the plaintiff's $1 million investment. The case, assigned to U.S. District Judge Vernon S. Broderick, is 1:24-cv-09918, Goldeneye Advisors, LLC v. Hanaco Venture Capital, Ltd. et al.
Who Got The Work
Attorneys from A&O Shearman has stepped in as defense counsel for Toronto-Dominion Bank and other defendants in a pending securities class action. The suit, filed Dec. 11 in New York Southern District Court by Bleichmar Fonti & Auld, accuses the defendants of concealing the bank's 'pervasive' deficiencies in regards to its compliance with the Bank Secrecy Act and the quality of its anti-money laundering controls. The case, assigned to U.S. District Judge Arun Subramanian, is 1:24-cv-09445, Gonzalez v. The Toronto-Dominion Bank et al.
Who Got The Work
Crown Castle International, a Pennsylvania company providing shared communications infrastructure, has turned to Luke D. Wolf of Gordon Rees Scully Mansukhani to fend off a pending breach-of-contract lawsuit. The court action, filed Nov. 25 in Michigan Eastern District Court by Hooper Hathaway PC on behalf of The Town Residences LLC, accuses Crown Castle of failing to transfer approximately $30,000 in utility payments from T-Mobile in breach of a roof-top lease and assignment agreement. The case, assigned to U.S. District Judge Susan K. Declercq, is 2:24-cv-13131, The Town Residences LLC v. T-Mobile US, Inc. et al.
Who Got The Work
Wilfred P. Coronato and Daniel M. Schwartz of McCarter & English have stepped in as defense counsel to Electrolux Home Products Inc. in a pending product liability lawsuit. The court action, filed Nov. 26 in New York Eastern District Court by Poulos Lopiccolo PC and Nagel Rice LLP on behalf of David Stern, alleges that the defendant's refrigerators’ drawers and shelving repeatedly break and fall apart within months after purchase. The case, assigned to U.S. District Judge Joan M. Azrack, is 2:24-cv-08204, Stern v. Electrolux Home Products, Inc.
Featured Firms
Law Offices of Gary Martin Hays & Associates, P.C.
(470) 294-1674
Law Offices of Mark E. Salomone
(857) 444-6468
Smith & Hassler
(713) 739-1250






