Why It's Time to Embrace Telehealth as the New Normal
While the concept of telemedicine may not be completely foreign, the experience of this medical care currently exists at the boundaries of the general (and legal) community. Nevertheless, as technology grows and continues to shrink the distances between us, so too have we seen the growth of telemedicine, and to a broader extent, telehealth.
April 07, 2020 at 05:15 PM
8 minute read
 MaryKate McGrath,left, and Adam J. Fulginiti, right, of Marshall Dennehey Coleman Warner & Goggin.
MaryKate McGrath,left, and Adam J. Fulginiti, right, of Marshall Dennehey Coleman Warner & Goggin.
As we begin to adjust to the new normal of life with COVID-19, be it through social distancing, avoiding large crowds and "hunkering down" with family, one issue thrust to the forefront is telemedicine—a relatively new type of medical practice that may help treat symptomatic individuals while stemming the spread of the coronavirus.
The experience of going to the doctor's office, either for a routine checkup or for the treatment of a particular condition, is one shared by millions of Americans. And to many, while the concept of telemedicine may not be completely foreign, the experience of this medical care currently exists at the boundaries of the general (and legal) community. Nevertheless, as technology grows and continues to shrink the distances between us, so too have we seen the growth of telemedicine, and to a broader extent, telehealth. With these new expansions, we also see the charting of a new legal frontier, through which telehealth and telemedicine are likely to be operated, regulated, and ultimately, litigated, in the coming years.
|A Primer on Basic Terminology and Application
In order to properly grasp the current (and future) legal issues surrounding the rapidly growing areas of telehealth and telemedicine, it is first necessary to understand the basic concepts that form the backdrop of this new landscape.
At the most basic level, the terms "telehealth" and "telemedicine" are typically differentiated according to the concept of patient care. While the specific definitions vary from state to state, telemedicine is generally considered a subset of telehealth. The latter consists of overall access to health information, which may, depending on the situation, involve the exchange of patient information, health-related education, data regarding public health and health care administration, and of course, the provision of clinical health care, all of which via some form of telecommunication medium. Telemedicine, on the other hand, is more specific, and deals primarily with the administration of individual patient care.
The methods of applying telehealth and telemedicine are inexorably tied to our technological and telecommunication capacities. Current delivery systems include two-way video (via laptop or desktop computer), email, and even handheld devices such as smart phones and tablets. Regardless of the method, the basic tenets include a "distant site," which pertains to the location of the physician or other licensed practitioner delivering the service, and the "originating site," the site of the patient or other individual who receives those services.
|Facilitating Access to Telemedicine
Given its ability to transcend county, state, and international borders, one of the legal "hurdles" facing telemedicine is the issue of medical licensure. Simply put, how can a physician at a distant site in Arizona, deliver telemedicine services to a patient at an originating site in West Virginia, Wisconsin or Maine? The answer, at least in part, can be found in an interstate agreement known as the Interstate Medical Licensure Compact, or IMLC.
At its core, one of the primary missions of the IMLC, and ultimately, telemedicine in general, is to "increase access to health care for patients in underserved or rural areas and allowing them to more easily connect with medical experts through the use of telemedicine technologies." To do this, the IMLC enables physicians to obtain licensure in multiple states, while obviating the need to submit separate applications to each individual state. At the same time, the IMLC provides protection to the public, by "enhancing states' ability to share investigative and disciplinary information."
The IMLC currently exists among twenty nine states, along with the District of Columbia and Guam. Once a physician becomes licensed in his or her home state (referred to in the IMLC as "principle location"), they can then apply for licensure in other participating states through "The Compact." As for Pennsylvania, the IMLC has already been passed and signed into law; however, implementation has been delayed due to logistics regarding information sharing.
Instructions regarding the application process, as well as the necessary criteria, are included within the IMLC's website. Current estimates project that approximately 80% of physicians in the United States meet the IMLC criteria, a factor that is likely to increase use of The Compact, and in turn, telemedicine services, in years to come.
|Regulation of Telehealth
Federal and state statutes address the intersection of health care and technology. The Health Insurance Portability and Accountability Act (HIPAA) and the Health Information Technology for Economic & Clinical Health Act (HITECH) provide specific protections for health data integrity, confidentiality and availability. The Patient Protection & Affordable Care Act (PPACA or the Affordable Care Act) provides oversight of the telehealth under the backdrop of the expansion of insurance coverage. The Medicare Access and CHIP Reauthorization Ac of 2015 (MACRA) incentivizes providers for efficient health care and improved outcomes, offering increased billing rates for specific services provided through telemedicine, and bonuses for implementing certain electronic billing and medical record programs.
Several states have already passed acts which specifically regulate the provision of health care through the use of technology, and within the next five years all U.S. states and territories are expected to have enacted formal telehealth legislation. Pennsylvania is currently on its second attempt to pass a Telemedicine Act, with efforts spearheaded by state Sen. Elder A. Vogel Jr. of Beaver, Butler and Lawrence counties. The initial legislative attempt of Senate Bill 780 sought to define key components of telemedicine and set licensing requirements. Senate Bill 780 was removed from table on Sept. 26, 2018, reportedly because the bill required parity in payment for telemedicine services, meaning that the payers, generally health insurers, would reimburse telemedicine services at the same rate as in-person services.
Pennsylvania Senate Bill 857, Vogel's second attempt at passing a Pennsylvania Telemedicine Act, was referred to the Rules and Executive Nominations Committee (Pennsylvania Senate) on Nov. 21, 2019. Like its predecessor, Senate Bill 857 proposes definitions for telemedicine and telehealth, while providing temporary guidelines regarding patient evaluation and treatment services. The proposed legislation gives state departments two years to draft permanent rules and regulations.
The prior legislative stumbling block regarding parity has been addressed with language which provides temporary ground rules for telemedicine reimbursement, without the specific requirement that telemedicine services must be compensated at a rate commensurate with in-person services. While a kick-the-can approach may be a necessary first-step in enacting a telemedicine statute in Pennsylvania, the parity issue will ultimately require resolution. Payers, providers and patients currently shy away from telemedicine offerings, simply in efforts to avoid the significant confusion which exists about whether care via telemedicine services should be recognized as equal, separate-but-equal or inferior to in-person care.
|What to Expect With Telehealth
Telehealth has been with us for longer than we may realize. Think back to 1895: if a physician diagnosed a fracture using the cutting-edge technology of an X-ray machine, then communicated those X-ray results to another physician via the slightly-older technology of a telephone, then those physicians were the "telemedicine pioneers" of their time. However, we are far from the days of Wilhelm Conrad Roentgen and Alexander Graham Bell.
Technology races forward, and how the law keeps pace is a decidedly open question. Courts throughout the United States have not been presented with many questions on telemedicine standards, nor about how the implementation of telemedicine may impact the provision of health care. Privacy issues have emerged, ranging from claims of improper acquisition and dissemination of protected health information in electronic format, to the alleged failure of a health care system employer to prevent a cyberattack on electronic systems containing employee protected health information.
As you read this article today, we are surrounded by uncertainty on several fronts, regarding the number of reported coronavirus cases, the availability of testing, shortages of basic medical supplies and the hunt for vaccines and treatment. We share concerns about taking loved ones for necessary medical treatment, for fear of COVID-19 exposure from another patient in a waiting room, a medical instrument, or even the medical provider who may unknowingly be carrying the virus. As we shelter in-place, we experience first-hand the benefits of a telemedicine consult where our primary care physician has the ability to perform a physical assessment over a smartphone or computer, or remotely monitor heart rates and blood glucose levels. Our "new normal" will hopefully prompt our lawmakers to enact comprehensive telehealth legislation, and facilitate increased patient reliance on effective and safe telemedicine practices.
Mary Kate McGrath, is a shareholder and chair of Marshall Dennehey Warner Coleman & Goggin's teleheath and telemedicine practice group in the Philadelphia office. Adam Fulginiti, an associate with the firm, is a member of the health care department. They may be reached, respectively, at [email protected] and [email protected].
This content has been archived. It is available through our partners, LexisNexis® and Bloomberg Law.
To view this content, please continue to their sites.
Not a Lexis Subscriber?
Subscribe Now
Not a Bloomberg Law Subscriber?
Subscribe Now
NOT FOR REPRINT
© 2024 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.
You Might Like
View All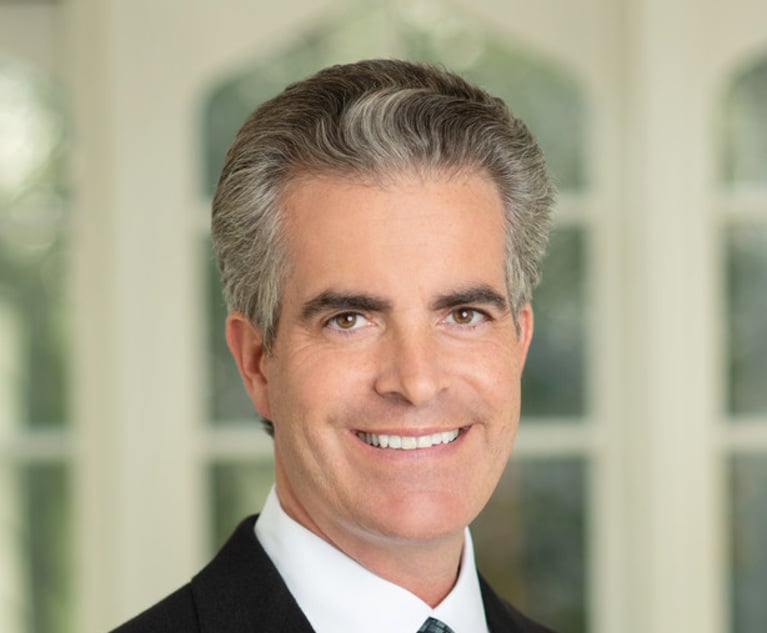
Pa. Hospital Agrees to $16M Settlement Following High Schooler's Improper Discharge
4 minute read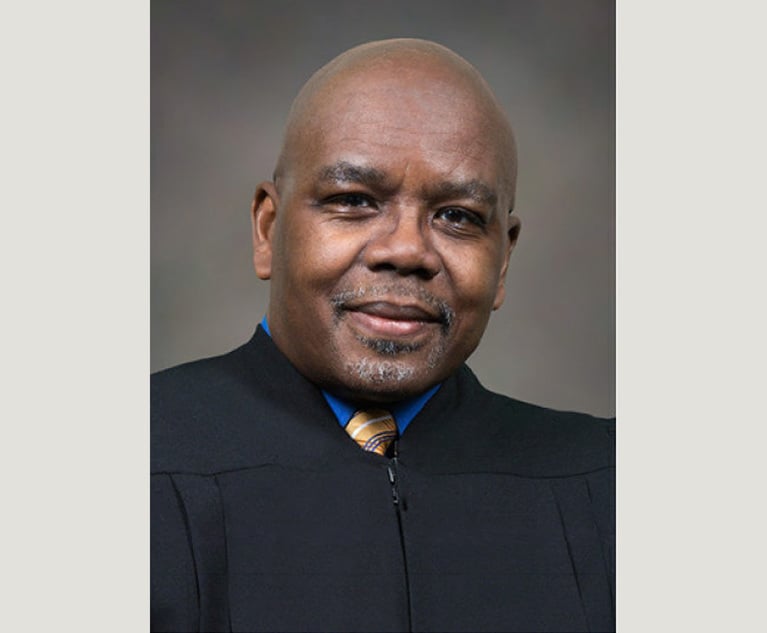
Plaintiffs Seek Redo of First Trial Over Medical Device Plant's Emissions
4 minute read
Hospital Must Provide Pre-Complaint Discovery in Privacy Breach Case, Pa. Judge Rules
4 minute read
Phila. Anesthesiologist Wins Defense Verdict in Multimillion-Dollar Case Over C-Section Complications
3 minute readLaw Firms Mentioned
Trending Stories
- 1Decision of the Day: Judge Reduces $287M Jury Verdict Against Harley-Davidson in Wrongful Death Suit
- 2Kirkland to Covington: 2024's International Chart Toppers and Award Winners
- 3Decision of the Day: Judge Denies Summary Judgment Motions in Suit by Runner Injured in Brooklyn Bridge Park
- 4KISS, Profit Motive and Foreign Currency Contracts
- 512 Days of … Web Analytics
Who Got The Work
Michael G. Bongiorno, Andrew Scott Dulberg and Elizabeth E. Driscoll from Wilmer Cutler Pickering Hale and Dorr have stepped in to represent Symbotic Inc., an A.I.-enabled technology platform that focuses on increasing supply chain efficiency, and other defendants in a pending shareholder derivative lawsuit. The case, filed Oct. 2 in Massachusetts District Court by the Brown Law Firm on behalf of Stephen Austen, accuses certain officers and directors of misleading investors in regard to Symbotic's potential for margin growth by failing to disclose that the company was not equipped to timely deploy its systems or manage expenses through project delays. The case, assigned to U.S. District Judge Nathaniel M. Gorton, is 1:24-cv-12522, Austen v. Cohen et al.
Who Got The Work
Edmund Polubinski and Marie Killmond of Davis Polk & Wardwell have entered appearances for data platform software development company MongoDB and other defendants in a pending shareholder derivative lawsuit. The action, filed Oct. 7 in New York Southern District Court by the Brown Law Firm, accuses the company's directors and/or officers of falsely expressing confidence in the company’s restructuring of its sales incentive plan and downplaying the severity of decreases in its upfront commitments. The case is 1:24-cv-07594, Roy v. Ittycheria et al.
Who Got The Work
Amy O. Bruchs and Kurt F. Ellison of Michael Best & Friedrich have entered appearances for Epic Systems Corp. in a pending employment discrimination lawsuit. The suit was filed Sept. 7 in Wisconsin Western District Court by Levine Eisberner LLC and Siri & Glimstad on behalf of a project manager who claims that he was wrongfully terminated after applying for a religious exemption to the defendant's COVID-19 vaccine mandate. The case, assigned to U.S. Magistrate Judge Anita Marie Boor, is 3:24-cv-00630, Secker, Nathan v. Epic Systems Corporation.
Who Got The Work
David X. Sullivan, Thomas J. Finn and Gregory A. Hall from McCarter & English have entered appearances for Sunrun Installation Services in a pending civil rights lawsuit. The complaint was filed Sept. 4 in Connecticut District Court by attorney Robert M. Berke on behalf of former employee George Edward Steins, who was arrested and charged with employing an unregistered home improvement salesperson. The complaint alleges that had Sunrun informed the Connecticut Department of Consumer Protection that the plaintiff's employment had ended in 2017 and that he no longer held Sunrun's home improvement contractor license, he would not have been hit with charges, which were dismissed in May 2024. The case, assigned to U.S. District Judge Jeffrey A. Meyer, is 3:24-cv-01423, Steins v. Sunrun, Inc. et al.
Who Got The Work
Greenberg Traurig shareholder Joshua L. Raskin has entered an appearance for boohoo.com UK Ltd. in a pending patent infringement lawsuit. The suit, filed Sept. 3 in Texas Eastern District Court by Rozier Hardt McDonough on behalf of Alto Dynamics, asserts five patents related to an online shopping platform. The case, assigned to U.S. District Judge Rodney Gilstrap, is 2:24-cv-00719, Alto Dynamics, LLC v. boohoo.com UK Limited.
Featured Firms
Law Offices of Gary Martin Hays & Associates, P.C.
(470) 294-1674
Law Offices of Mark E. Salomone
(857) 444-6468
Smith & Hassler
(713) 739-1250





